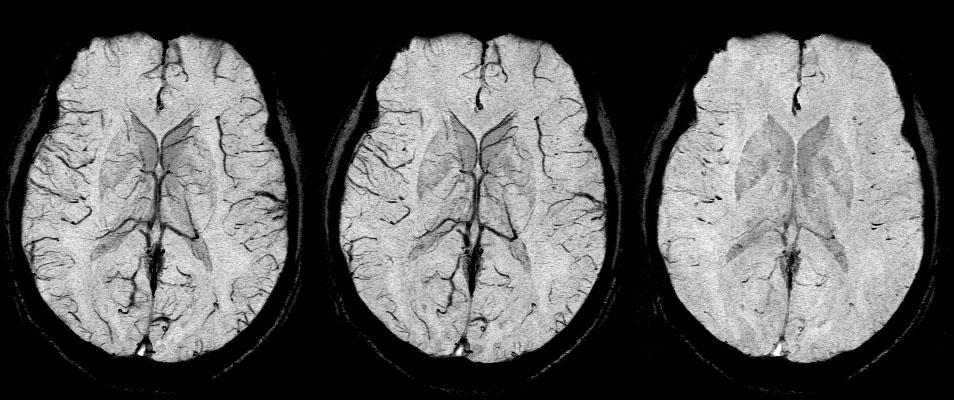
SWI examples
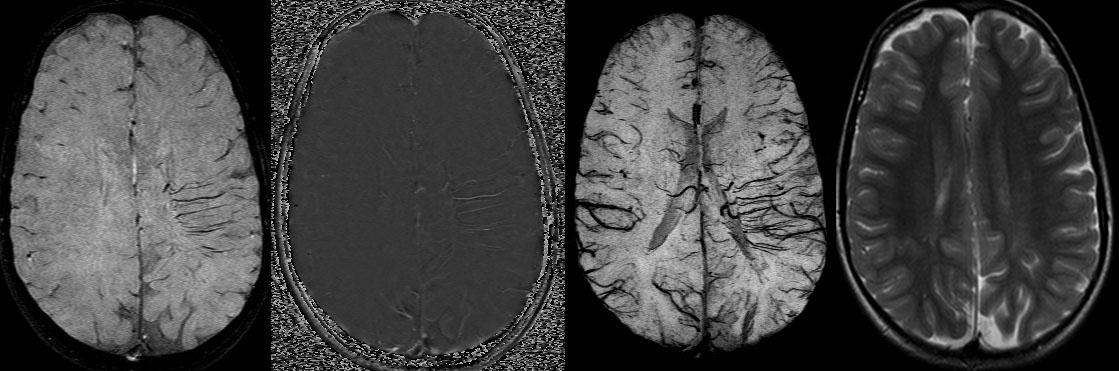
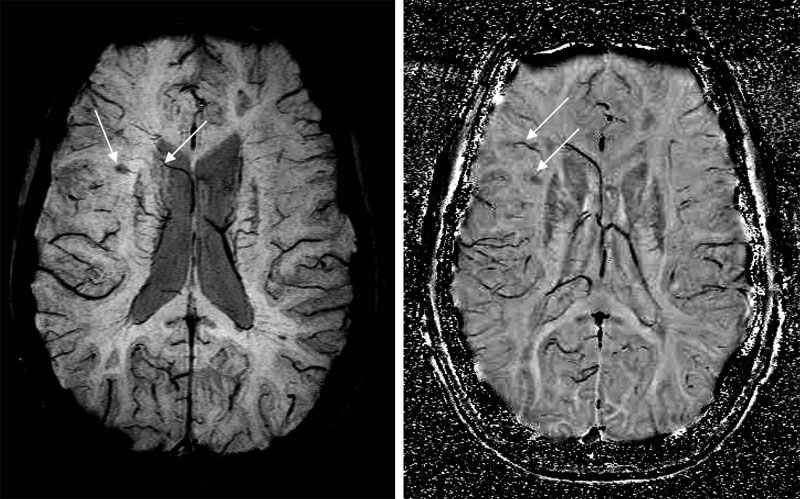
Slices of SWS patient showing deep white matter or medullary veins:
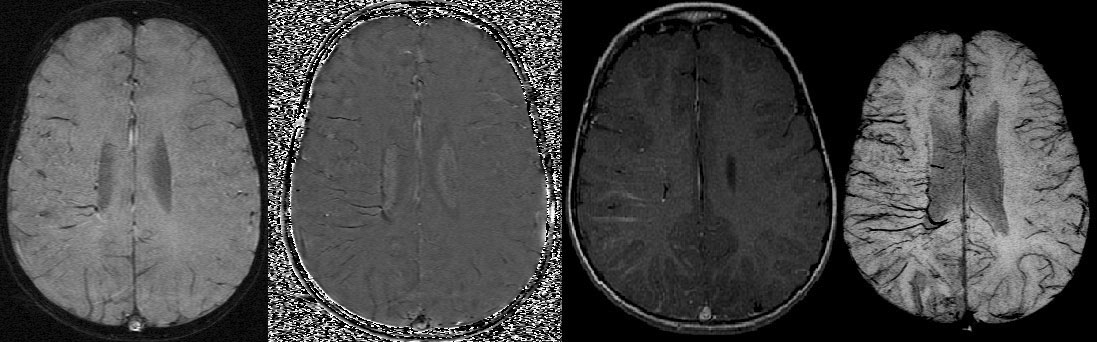
Trauma for Both Adults and Children(acquired at 1.5T):
-Diffuse axonal injury:
-Hemorrhage:
Stroke and Hemorrhage(data acquired at 1.5T):
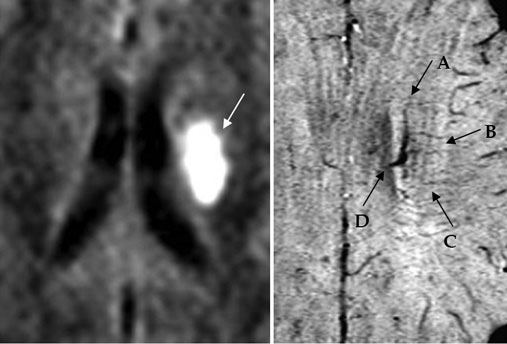
The arrows in the SWI image may show the tissue at risk that has been affected by
the stroke (A, B, C) and the location of the stroke itself (D).
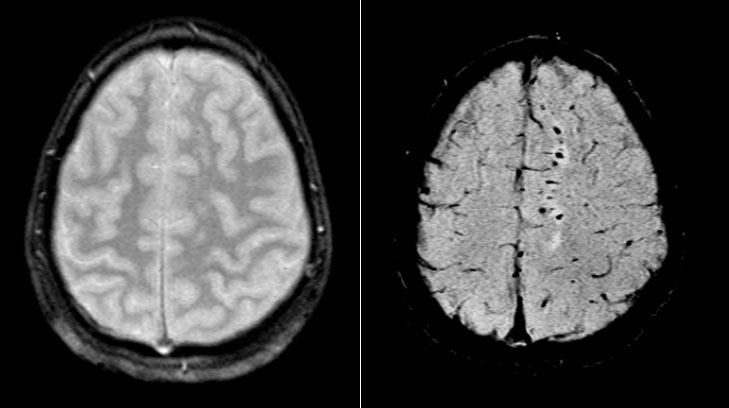
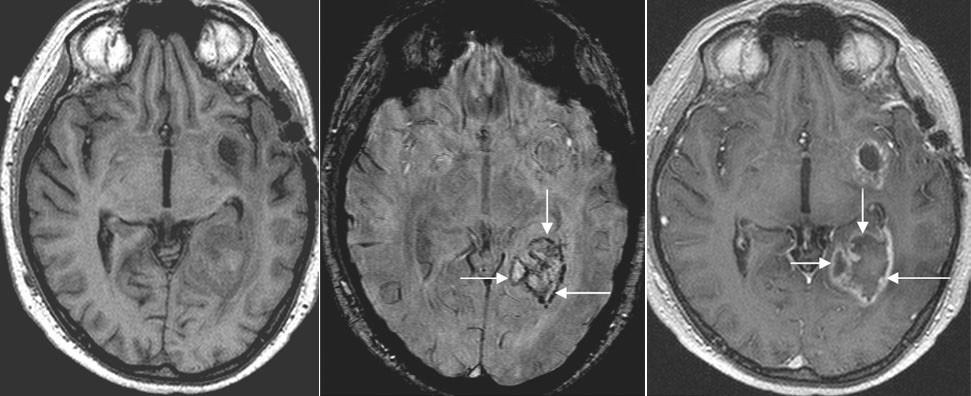
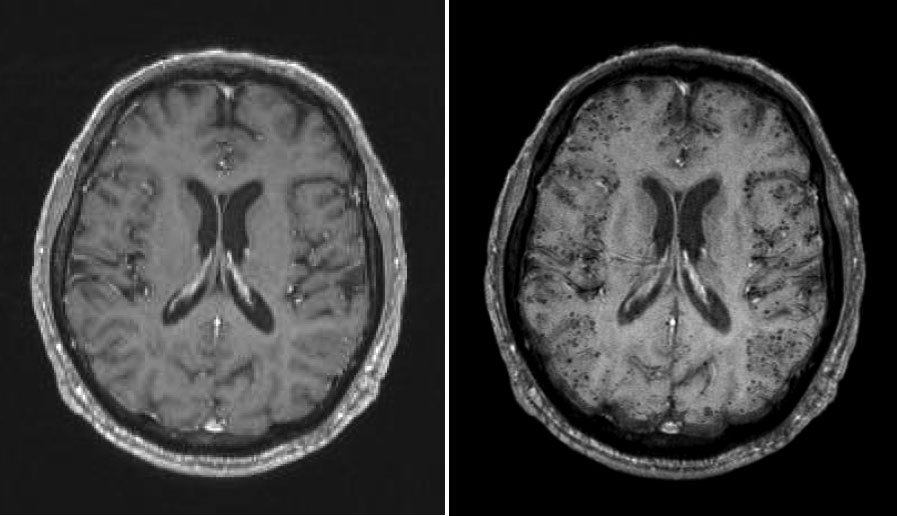
Sturge-Weber Disease:
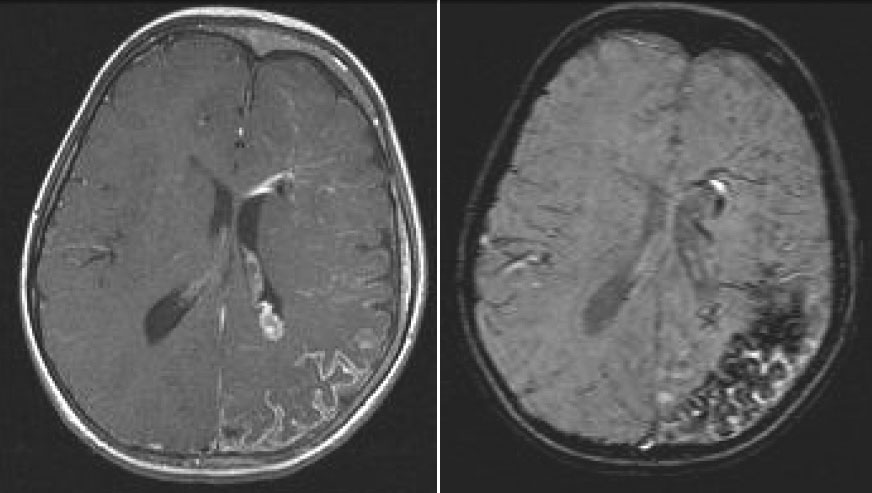
-first image: Contrast enhanced T1 weighted imaging showing the leptomeningeal enhancement present in Sturge-Weber disease.
-second image: Post-contrast SWI showing a markedly hypointense region in the underlying white matter that could ref lect increased deoxyhemoglobin, increased local venous blood volume and/or calcification.
Tumor:
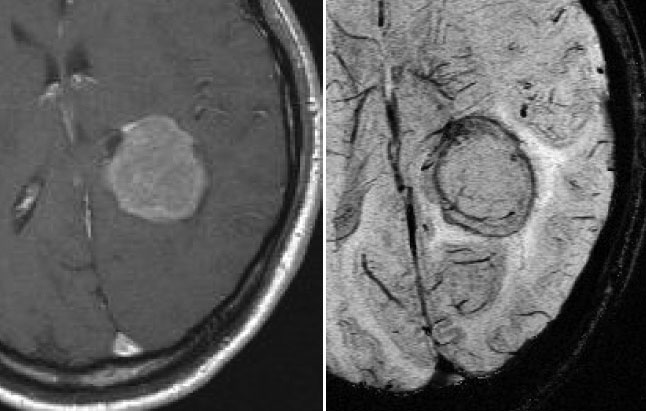
![]() T1 Post-Contrast
T1 Post-Contrast
![]() SWI
SWI
![]() T1 Post-Contrast
T1 Post-Contrast
![]() SWI
SWI
Visualizing Oxygen Saturation in Tumors:
Breathing normal air has a better visualization of the veins (left image) than breathing oxygen (middle image) because of the higher deoxyhemoglobin lack. On the other hand, carbogen (5% CO2, 95% O2) breathing induces an increase in venous blood oxygenation which leads to a reduction of field inhomogeneities around the vessels. Consequently, the contrast between veins and surrounding parenchyma is reduced (right image).
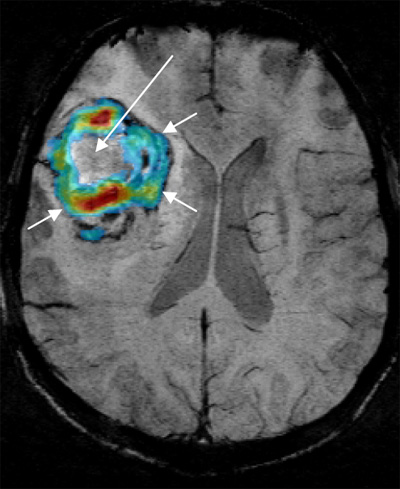
Venogram of a tumor patient with the overlaid SWI signal increase during carbogen breathing. Tumor response to carbogen breathing is spatially heterogeneous with an inactive necrotic tumor center (long arrow) and an active periphery (short arrows).
Tumor Boundaries with SWI:
Detection of Hemorrhage in Tumors with SWI:
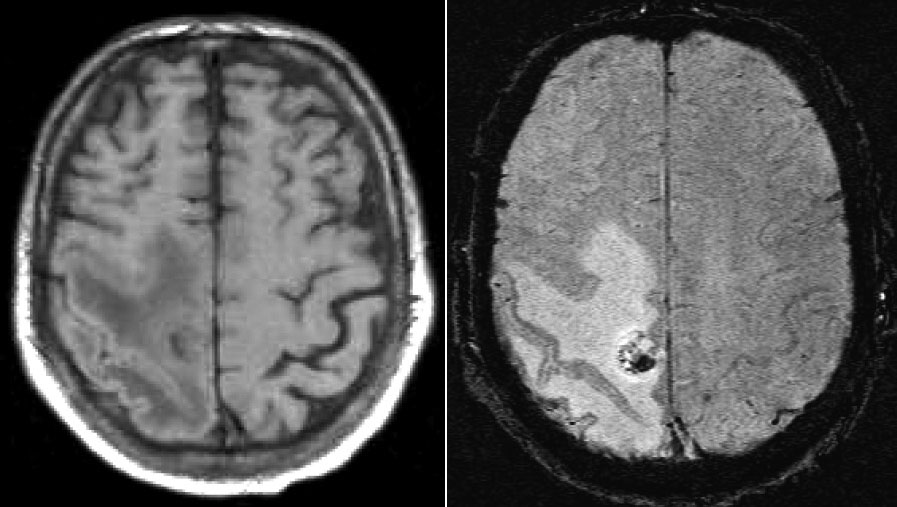
First image: A pre-contrast T1 weighted scan of a brain metastasis which doesn't show any hint of hemorrhage.
Second image: Using the SWI method, there is evidence of blood products which have been confirmed by pathology.
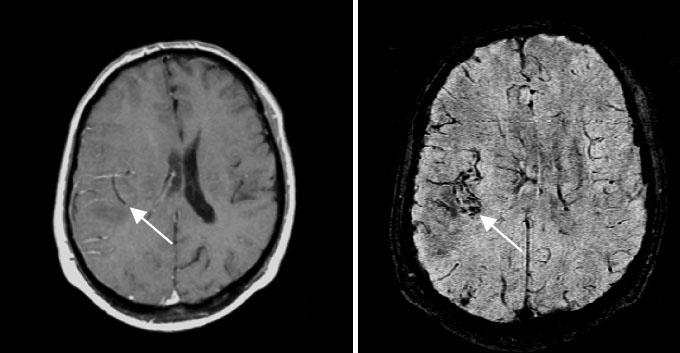
Multiple Sclerosis:
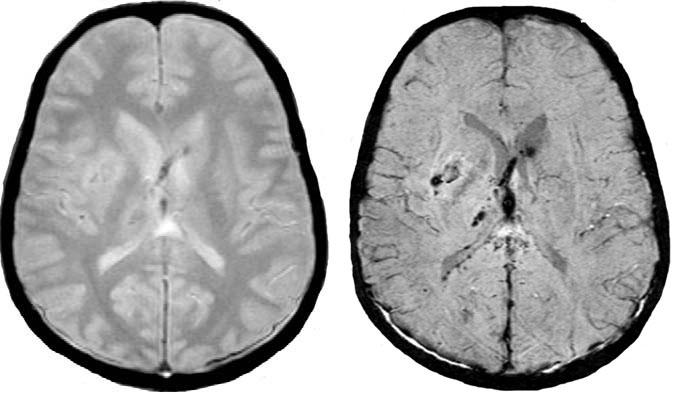
Vascular Dementia and Cerebral Amyloid Angiopathy (CAA):
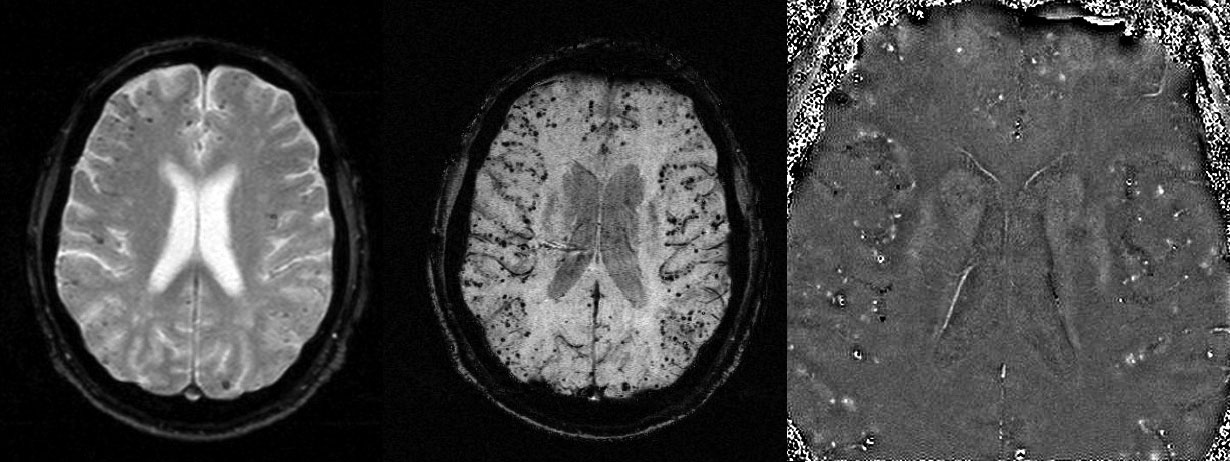
T1-weighted image (left) and overlay of the SWI image on the T1 image (right), showing
that CAA in this patient is ubiquitous in the parenchyma.